If you’ve been following Covid news, then you’re likely well aware there’s a new variant in town that’s concerning the scientific community.
Known as XBB, the variant is believed to be the most immune-evasive to date and currently accounts for over 40% of infections in the United States, according to data from the US Centers for Disease Control and Prevention.
Advertisement
It’s been called the “kraken variant” by some, and according to the World Health Organisation, it has now been identified in at least 28 other countries.
As the BBC reported, some cases of XBB.1.5 variant, which evolved from XBB, have already been recorded in the UK – the mutation helped it beat the body’s immune defences, but has also reduced its ability to infect human cells, the report said.
Because XBB is relatively new, scientists are still working to figure out if and how the variant behaves differently from other recent variants. Though XBB’s symptoms are expected to be on par with past omicron infections, doctors say they are seeing some issues becoming more prevalent than others.
“Viruses typically mutate to become more contagious and less severe; it appears that this is happening with this strain of the coronavirus,” Dr. Henry Redel, the chief of infectious disease at Saint Peter’s University Hospital in New Brunswick, New Jersey, tells HuffPost US.
Advertisement
We asked infectious disease experts what they’re seeing in US hospitals right now. Here’s what they said.
The most common XBB Covid symptoms appear to be congestion and body aches.
There’s limited data on XBB, but experts suspect the symptoms associated with XBB infections will be similar to the symptoms people experienced with Covid throughout 2022.
That said, evidence has shown that the symptom profile has shifted a bit with each variant. Omicron caused more cold-like symptoms (like fatigue, runny nose, sneezing and muscle aches), for example, whereas delta and alpha more commonly triggered anosmia (loss of smell) and ageusia (loss of taste).
So, what is on the docket for XBB? “In general, I think people are more achy and still have congestion and headache,” Dr Julie Parsonnet, an infectious diseases specialist with Stanford Health Care, tells HuffPost. You may also expect to see the other usual symptoms: fever, chills, cough and sore throat.
Less common symptoms include loss of taste and smell and shortness of breath.
Anosmia and ageusia appear, anecdotally, to be less common with XBB. Experts don’t expect ageusia and anosmia to make a comeback just yet.
Advertisement
“Since XBB is part of the Omicron group, I expect that loss of taste and smell will not be common, but I have not seen data yet,” says Dr. Thomas Campbell, a professor in the department of infectious disease at the University of Colorado Anschutz Medical Campus.
One thing doctors on the front lines are seeing less of: severe shortness of breath, Redel says. Rarely have recent patients needed supplemental oxygen, he added. Redel notes he’s seeing many more Covid patients come in with classic upper respiratory symptoms – like runny nose, congestion and sore throats – along with fever and muscle aches.

Malcolm P Chapman via Getty Images
What causes symptoms to change between subvariants?
Because so many people have been infected – in some cases, multiple times — it’s tough to pin down exactly how the symptomatology is influenced by the host versus specific traits of the virus. Parsonnet suspects that immunity plays a pretty big role.
“There is likely a strong element of underlying immunity, but there may also be differences in the virus’s ability to cause symptoms,” Parsonnet tells HuffPost.
Advertisement
According to Dr. Martin Krsak, an infectious disease expert at the University of Colorado Anschutz Medical Campus, people’s genetics and underlying health – i.e. whether they have a chronic disease or prior injury – also influence the type of symptoms they develop.
Like Parsonnet, Krsak says that each variant and the way it infects our cells likely impacts symptoms as well. “Variants have a different capacity to evade prior immunity and also a different capacity to bind to the main target on human cells,” he says.
Does the current Covid booster prevent you from getting infected with XBB?
A pre-print study from Japan determined that XBB came to be during the summer of 2022 when two sub-variants of the BA.2 omicron lineage combined. Scientists believe that, in this process, XBB picked up mutations that help it better evade immunity conferred by both vaccination and previous infections.
XBB’s mutations also let it attach to our cells more easily, enabling it to spread more efficiently than other versions of omicron.
“It binds tighter, appears more transmissible, and is also immune-evasive,” says Dr. Eric M. Poeschla, the head of the Division of Infectious Diseases at the University of Colorado Anschutz Medical Campus. It’s unknown whether those mutations alter the virus’ clinical profile and the symptoms it causes, Parsonnet says.
Advertisement
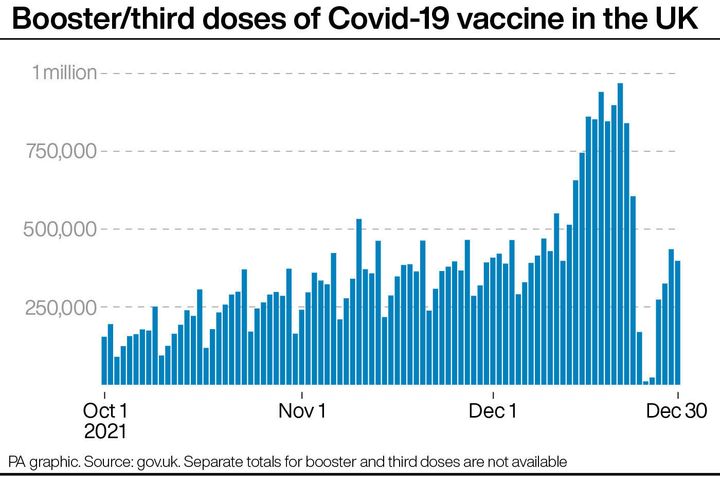
The updated Covid booster, which was tweaked in 2022 to target newer variants of Omicron, doesn’t work super well at preventing infections of XBB, considering there are so many new infections in the community, Parsonnet says.
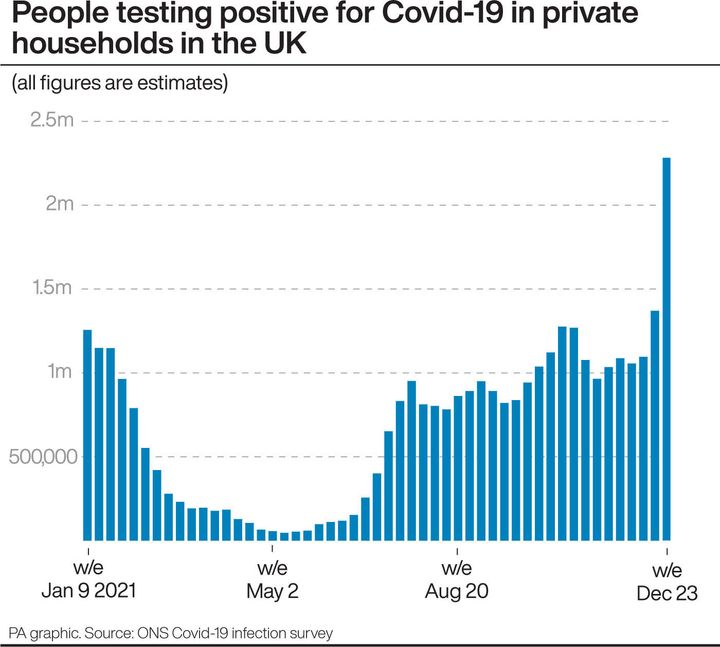
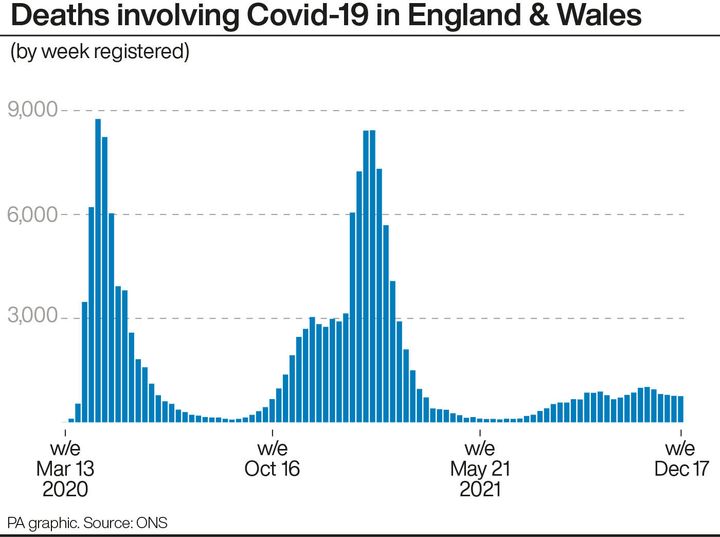
But the fact that there hasn’t been a rapid increase in deaths shows that the shots, combined with the immense amount of immunity gained from past infections, continue to protect many people from severe outcomes. Together, that immunity will help blunt the XBB wave, according to Poeschla.
Of course, there’s always the very real risk of long Covid, which is a debilitating condition that can follow even a mild case of the coronavirus. Long Covid can cause lasting fatigue, brain fog, respiratory issues and more. There’s still a lot for us to learn about XBB and the symptoms or potential complications it may cause.
But there’s one thing we know for sure: There’s a benefit to being vaccinated rather than not. “The bivalent booster offers some protection against all omicron-based variants and is highly recommended, especially for those over 65 or with serious other risks,” Poeschla says.
Experts are still learning about Covid-19. The information in this story is what was known or available at the time of publication, but guidance could change as scientists discover more about the virus. To keep up to date with health advice and cases in your area, visit gov.uk/coronavirus and nhs.uk.
Advertisement