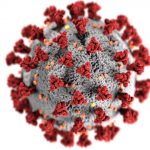
 I used to joke that for all the hardships of being a physician, at least we had job security. Little did I know that a viral illness would put some physicians “on the bread line.”
I used to joke that for all the hardships of being a physician, at least we had job security. Little did I know that a viral illness would put some physicians “on the bread line.”
The COVID-19 pandemic has negatively impacted the physician workforce in both anticipated and unanticpated ways. While stay-at-home orders decrease temporary demand for cosmetic and elective surgical procedures by dermatologists and orthopedic surgeons, inpatient rehabilitation facilities are also feeling the squeeze, though the number of patients who need their services are growing exponentially (due to post-COVID syndromes).
In states of emergency, hospitals at (or over) capacity have the right to commandeer beds from other units within their system. So for example, if there is a unit devoted to the rehabilitation of stroke or car accident victims, the hospital might re-allocate those beds to COVID-19 patients. There is also financial incentive to do so because Medicare pays 20% higher rates to hospitals for each COVID patient that requires admission.
So what happens when the rehab unit turns into a COVID unit? A few things. First, the patients who need inpatient rehabilitation with close physician monitoring are turfed to nursing homes. Fragile stroke patients, those with high risk for neurological or cardiac decompensation, and inpatients with complex medical problems (such as internal bleeding, kidney failure, or infectious diseases) are sent to a lower level of care without suficient oversight by physicians. These patients often crash, get readmitted to the hospital, or in the worst case, decline too quickly to be saved.
Second, the physicians who take care of rehab patients (rehabilitation physicians, also known as physiatrists) hand over care of the COVID patients (in the former rehab unit) to hospitalists, reducing their own workloads substantially while the hospitalists are overwhelmed and at risk for burn out.
Third, hospitals are struggling to cut costs due to the suspension of their lucrative elective surgical pipelines during COVID surges – and put a moratorium on hiring additional physicians who would normally be assisting with growth and expansion efforts in neuromuscular, brain and spinal cord injury rehabilitation.
Finally, in some cases rehab units are experiencing low censuses not because their beds were commandeered for COVID patients, but because elective surgeries have diminished and patients are afraid of coming to the hospital. Many of those with symptoms of heart attacks, strokes, brain injuries, etc. are staying home and “gutting it out” while reversible or treatable injuries and disabilities become permanent. The devastating toll will be difficult to quantify until normal medical surveillance and care resumes.
Meanwhile, physiatrists with outpatient practices and pain management clinics are experiencing a dramatic drop in patient throughput, with telemedicine visits largely inaccessible to the poor and disabled populations they serve. Those outpatient physicians seek to augment their income with part-time inpatient work, and unprecidented numbers are seeking employment through locum tenens agencies. Unfortunately, agencies have scant inpatient jobs to offer for the reasons I discussed above, and competition is fierce among agencies and physicians alike. It’s often the case that 7 or more agencies will contact a physician within hours of a new job posting, and that job will be filled before the physician can respond – and at an hourly rate 20-30% lower than pre-COVID days (based on my personal experience).
These are some of the unexpected underemployment consequences of the COVID pandemic for one sub-specialty group: physiatry. I imagine the forces at play may be similar for my peers in oncology, neurology, or preventive medicine, for example.
One thing is for sure: emergency medicine physicians, internists, and critical care specialists are facing a tsunami of patients while others of us are sitting on the bench, wanting to help but not trained to do so, “sheltering in place” as the non-COVID march of disease and disability continues apace.


 Medical school prepares physicians to prescribe medications for prevention and treatment of disease, but little to no time is spent teaching something just as important: de-prescribing. In our current system of auto-refills, e-prescriptions, and mindless “check box” EMR medication reconciliation, patients may continue taking medications
Medical school prepares physicians to prescribe medications for prevention and treatment of disease, but little to no time is spent teaching something just as important: de-prescribing. In our current system of auto-refills, e-prescriptions, and mindless “check box” EMR medication reconciliation, patients may continue taking medications  Rehabilitation medicine is one of the best-kept secrets in healthcare. Although the specialty is as old as America’s Civil War, few people are familiar with its history and purpose. Born out of compassion for wounded soldiers in desperate need of societal re-entry and meaningful employment, “physical reconstruction” programs were developed to provide everything from adaptive equipment to family training, labor alternatives and psychological support for veterans.
Rehabilitation medicine is one of the best-kept secrets in healthcare. Although the specialty is as old as America’s Civil War, few people are familiar with its history and purpose. Born out of compassion for wounded soldiers in desperate need of societal re-entry and meaningful employment, “physical reconstruction” programs were developed to provide everything from adaptive equipment to family training, labor alternatives and psychological support for veterans.