 Because science is advancing our understanding of medicine at an exponential rate, physicians and surgeons have been turning to subspecialization as a means to narrow their required domains of expertise. “Carving out a niche” makes sense in a profession where new research is being published at a rate of two million articles per year. Just filtering the signal from the noise can be a full time job.
Because science is advancing our understanding of medicine at an exponential rate, physicians and surgeons have been turning to subspecialization as a means to narrow their required domains of expertise. “Carving out a niche” makes sense in a profession where new research is being published at a rate of two million articles per year. Just filtering the signal from the noise can be a full time job.
However, the consequences of narrowing one’s expertise is that you lose flexibility. For example, an orthopedist who has subspecialized in the surgical management of the shoulder joint doesn’t keep her skills sharp in knee replacement surgery or other general surgical procedures that she once performed. Neurologists who focus on movement disorders become comfortable with a small subset of diseases such as Parkinson’s, but then close their doors to patients with migraines or strokes.
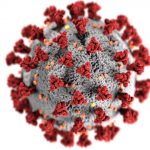
The continued march towards ultra-subspecialization has been a boon in urban and academic centers, but has left spotty expertise in surrounding areas and small towns. And now, the COVID-19 pandemic has unmasked the biggest downside of niche medicine: a hardening of the categories that prevents many physicians from being able to help in times of crisis. Retina specialists, plastic surgeons, rheumatologists, and radiation oncologists (to name just a few) may want to help emergency medicine physicians (EM), internists (IM), and intensivists (CCM) expand their reach as COVID cases surge and hospitals become overwhelmed. But what are they to do? They are not trained to manage airways, place central lines, or monitor renal function, and legitimately fear legal repercussions should they attempt to do so.
Medicine is fundamentally based upon apprentice-style learning – this is why we undergo years of residency training – to stand shoulder-to-shoulder with more senior experts and learn their craft under close supervision. Upon graduation from medical school, physicians are deemed ineligible to treat patients until they have practical experience under their belts. The old adage: “see one, do one, teach one” is the bedrock of how we train. So now, there needs to be a pathway available for those who have completed residency to re-train to meet the demands of this crisis and others.
Perhaps it’s a radical idea to consider pairing subspecialist physicians with current frontline COVID-19 doctors – but turfing patients to “non physician practitioners” or NPPs when access is limited to an emergency medicine specialist, internist, or intensivist, seems to be the current plan. I believe that medical school and internship are a solid foundation for COVID management (common to all physicians), and that given a designated EM, IM, or CCM mentor, the willing subspecialists will be able to follow protocols and take on new challenges rapidly and with excellence. I hope that the government will issue more detailed “good Samaritan” type laws to protect mentors and their subspecialty partners from frivolous law suits in times of COVID (those in place are for volunteer positions only), and that the house of medicine, led by the AMA and other sub-specialty organizations, will pave the way for rapid cross-disciplinary instruction and certification.
Going forward, there should be opportunities for post-residency, mid-career physicians to complete fellowship programs outside of their sub-specialty’s usual offerings. An ophthalmologist should have the ability to spend a year studying pulmonary medicine, for example, if they want to moonlight with an ICU physician in the future. In our current system, it is very difficult to obtain a fellowship after significant time has elapsed since one’s residency training. While there are a few “re-entry programs” for physicians who haven’t practiced clinical medicine for years, there is no path established for those who simply wish to switch specialties or assist outside of their specialty in a time of crisis.
I am not arguing that a fellowship should be considered equivalent to a residency program. We may need to create a new type of physician certification that allows fellowship-trained physicians from unrelated residency programs to operate under the license of an agreeable mentor/sponsor already established in the field by virtue of medical school and residency training. This would open up employment opportunities for over-specialized physicians, while not threatening those who are residency-trained in the field. In essence, this would allow physicians to operate in the way that NPPs have been for decades, and get subspecialty physicians off the bench and into the fight against COVID and perhaps into underserved areas more effectively as well.
For those subspecialists who have become disillusioned with their field, but still enjoy medicine or surgery – their talent could be retained if there were a path to re-training. An estimated 20% of physicians would change their specialty if they could. Currently, physicians have few clinical options if they no longer wish to practice in the field in which they completed a residency. I suspect that sweeping physician burnout rates (highest among mid-career physicians) could be improved by providing opportunities for “reimagining” themselves – and course-correcting to rekindle the scientific and clinical passion that led them to apply to medical school in the first place.
This would require some mental and regulatory flexibility – which could be a good side effect of the otherwise dreadful COVID pandemic.


 I used to joke that for all the hardships of being a physician, at least we had job security. Little did I know that a viral illness would put some physicians “on the bread line.”
I used to joke that for all the hardships of being a physician, at least we had job security. Little did I know that a viral illness would put some physicians “on the bread line.”









 American healthcare reform debates are focused on strategies to provide “access” to medical services for all. Lack of insurance (or under-insurance) seems to be the
American healthcare reform debates are focused on strategies to provide “access” to medical services for all. Lack of insurance (or under-insurance) seems to be the  Medical school prepares physicians to prescribe medications for prevention and treatment of disease, but little to no time is spent teaching something just as important: de-prescribing. In our current system of auto-refills, e-prescriptions, and mindless “check box” EMR medication reconciliation, patients may continue taking medications
Medical school prepares physicians to prescribe medications for prevention and treatment of disease, but little to no time is spent teaching something just as important: de-prescribing. In our current system of auto-refills, e-prescriptions, and mindless “check box” EMR medication reconciliation, patients may continue taking medications  I receive a significant amount of email in response to
I receive a significant amount of email in response to