Jake* was having an ordinary family meal with his partner and 15-year-old son when he came down with a fever. For four days he felt exhaustion and had no appetite at all, and after a few days he developed brain fog. Twenty-four hours later, an anal lesion appeared.
“It was essentially an open wound for five days which was emitting a clear mucus and then blood,” Jake tells HuffPost UK.
Advertisement
“It was almost impossible to sit down and moving was very painful. Opening my bowels was pure agony and my body was making me do that eight or nine times a day. Each time was a bloodbath.”
It was late July when the World Health Organisation (WHO) declared monkeypox a world health emergency.
The US Centers for Disease Control and Prevention (CDC) has estimated there are more than 25,000 cases worldwide – predominately in Europe, though more than 7,000 in the US, and more emerging in South America, South East Asia, the Western Pacific and the Eastern Mediterranean.
Advertisement
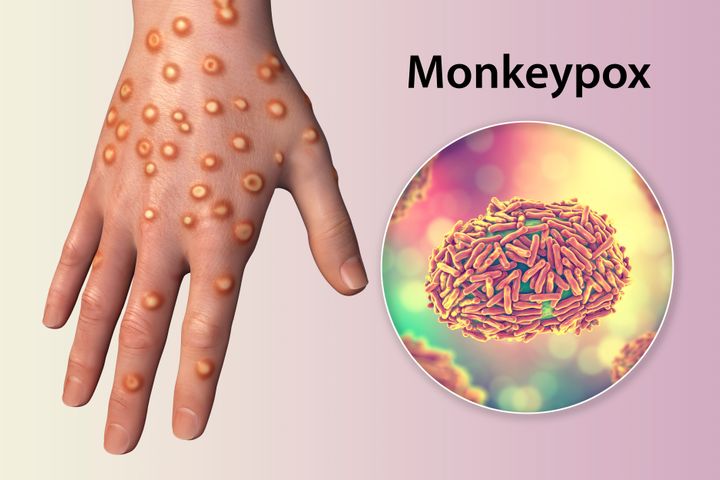
The virus was first reported in humans in 1970 in the Democratic Republic of Congo, having been identified in monkeys in a Danish laboratory in 1958 (thus the name). However, prior to 2021, there had only been seven UK cases.
As of August 4, there are more than 2,700 confirmed monkeypox cases in the UK, according to government figures, most in England and “a significant majority” of those – as many as 75% – in London.
Its prior rarity means knowledge of transmission among health experts is still patchy while we await more research – a period of stasis that echoes the early stages of Covid-19.
But this week, groups from across the political spectrum in Westminster joined forces, signing a letter to health secretary Steve Barclay calling for action on a disease that’s “causing real fear and anxiety” within queer communities.

FG Trade via Getty Images
While it’s possible for anyone, including children, to catch monkeypox, 98% of current cases are in men who identify as gay or bisexual, or men who have sex with men. This was confirmed by Dr Tedros Adhanom Ghebreyesus, director general of WHO, and he advised men to reduce their number of sexual partners while health authorities tackle the outbreak.
Advertisement
For decades, queer men have been subjected to unfair stigma around sexual promiscuity, particularly during the AIDS pandemic, and the lack of knowledge around the rise of monkeypox has obvious parallels with AIDS for those that remember the height of that crisis.
“We need to calmly and responsibly acknowledge that this current monkeypox outbreak is predominantly affecting gay and bisexual men.”
– Greg Owen, PrEP lead at Terrence Higgins Trust
So campaigners says it’s crucial that messaging about monkeypox transmission and vaccination is handled sensitively to avoid spreading further stigma against the LGBTQ+ community.
“We need to calmly and responsibly acknowledge that this current monkeypox outbreak is predominantly affecting gay and bisexual men,” says Greg Owen, PrEP lead at the Terrence Higgins Trust.
“We need to acknowledge that it’s also mainly being spread through the skin to skin contact, which is occurring during sex. There is nothing wrong with stating that. It is very problematic if we don’t.”
Advertisement
Dr Mark Lawton, a sexual health and HIV consultant in Liverpool and chair of the British Association of Sexual Health and HIV (BASHH), adds the following caution: “We believe, in addition to direct skin to skin to contact, monkeypox can be transmitted through contact with contaminated clothing and bedding and by respiratory droplets in close proximity.”
Harun Tulunay, a 35-year-old training coordinator who works with HIV/AIDS charity Positively UK, contracted a serious case of monkeypox in June.
“I was feeling like someone was ripping my flesh out of my bones,” says Tulunay of his experience. The Londoner doesn’t believe he developed monkeypox having sex, but through bodily touch, simply by lying next to a partner.
During his stint in hospital, the pain was so severe that doctors gave him opioids in an attempt to control the discomfort.

Harun Tulunay
Advertisement
“I wasn’t able to swallow, it was that bad,” he tells HuffPost UK. “The pain was worse than kidney stone pain. When they gave me antibiotics I was crying and kicking my bed and the doctors were holding me.”
While most monkeypox cases are much milder, there can be mental health implications for those who catch the virus.
Jake had been in close contact with his 80-year-old father in the period before his symptoms began and that, after getting a diagnosis, having to tell his family they might be at risk too gave him extra stress.
“Mentally it was very difficult,” says the professional services manager, who is bisexual, in his forties, and based in London.
“It meant my father knowing I’m in an open relationship which was stressful to share. My 80-year-old father has up until now just about managed to deal with my bisexuality by addressing it as little as possible. Now he is being contacted with offers for a vaccine as he may have been exposed.”
Advertisement

Twitter/@MonkeyPoxJake
The Department of Health & Social Care (DHSC) says it is working “rapidly” to vaccinate those at risk.
Vaccinations began in July, using Imvanex – a vaccine designed for smallpox – and NHS England has confirmed that 14,000 people have already received a jab, although priority is being given to those at higher risk of contracting it.
“It’s important to emphasise that vaccination will not give instant protection against infection or disease, and can take several weeks,” the WHO director-general said on July 27. “That means those vaccinated should continue to take measures to protect themselves, by avoiding close contact, including sex, with others who have or are at risk of having monkeypox.”
The US virus declared the virus a public health emergency on Thursday. For those confirmed to have monkeypox, the US CDC is recommending a two-to-four-week isolation period.
Advertisement
Now campaigners are calling for similar focus in the UK. Greg Owen is among many spokespeople for queer organisations putting pressure on the government to do more to control the spread of the virus and speed up vaccine roll-out.
“We want to see a national lead appointed to hold all of those in the fragmented system to account in terms of tackling the monkeypox outbreak with the ultimate goal of preventing it from becoming endemic in the UK,” he tells HuffPost UK. Owen believes we “urgently” need to double the amount of vaccines with “an injection of cash, quickly” put into sexual health services.
The open letter signed by Conservatives, Labour, Liberal Democrat, Green and Scottish National Party representatives, as well as charities. echoed this: “We are united as LGBT+ groups from across political parties in asking that the government treat the monkeypox outbreak as a public health emergency.”
Alongside the Terrence Higgins Trust and BASSH, the British HIV Association, PrEPster and the National AIDS Trust are also rallying for government action, including £51m funding from the Department of Health and Social Care.
The call is repeated by Dr Lawton: “Crucial to this is immediate mobilisation of resources by the government to ensure sexual health clinics, who are bearing the brunt of this, are funded to deal with the additional workload and sufficient vaccine is made available for all those that need it,” he tells HuffPost UK.
Advertisement
The Terrence Higgins Trust has also expressed concern that access to other vital healthcare support is being stretched due to health workers being overworked and having to focus on an influx of monkeypox patients.
“Some [sexual health services are] seeing a 90% reduction in access to the HIV prevention pill PrEP and long-acting reversible contraception,” the charity writes on its website.

Anna Bizon via Getty Images
Similarly to the early days of Covid-19, monkeypox is affecting people that are otherwise fit and healthy.
“I have no underlying health conditions,” says James,* who is 36, and asked to stay anonymous. “I work out six times a week and my fitness and health is my top priority. So for this to floor me the way it did, it was really scary. I also found the isolation really difficult, three weeks from the first sign and symptom is really tough!”
Advertisement
Meanwhile, John Thomas only experienced mild symptoms, but believes one of the major challenges is convincing men who have non-severe cases to isolate for the benefit of others.
“I think mild cases go under reported compared to the horror stories,” he tells HuffPost UK. “If you don’t know you have monkeypox, or if you can get away without people knowing you have it, you’re free to spread the virus to others.”
He adds: “If I hadn’t been looking for symptoms I would have almost certainly gone to a club night on the Friday [around the time of his transmission], and probably on the Saturday night as well.″ I think enough isn’t known about transmission yet, or if it is, the messaging is confusing.”
Thomas is right to have thought twice about going clubbing, says Dr Lawton, who says it is possible that monkeypox could spread in an intense nightclub environment where people are wearing little clothing.
“This is certainly a potential source of infection,” he says. “It is predominantly transmitted through skin to skin contact, but this does not need to be sexual.”
Advertisement
While we wait for more research, campaigners like Owen are trying to stay pragmatic.
While expressing “huge concerns,” including fears around vaccine equity, he tells HuffPost UK: “I tend not to ‘worry’ – worrying can be really debilitating.”
* Some names have been changed and surnames changed to offer anonymity.