While driving a year or so ago, social psychologist Rotem Kahalon began thinking about the words women use to describe their vagina.
Well, it wasn’t out of nowhere. Kahalon had been listening to a podcast on women’s health where a gynaecologist noted – almost in passing – that she was often surprised by how even older women refer to their genitalia using euphemisms such as “down there” or “pee-pee”.
Advertisement
“This remark struck me as potentially meaningful: it seemed likely to reflect how women perceive and relate to their genitalia, with possible implications for health-related behaviours and sexual pleasure,” said Kahalon, who’s an assistant professor in the faculty of medicine at Bar-Ilan University in Ramat Gan, Israel.
For instance, does using more anatomically correct language like “vagina” or “vulva” increase your enjoyment of sex? What effect does using dirty talk like “pussy” have on body image? And what about our mothers and grandmothers, who on the whole, vastly prefer “privates” or “pee pee”?
Turns out, the terms you use to describe your nether regions (there’s a euphemism for you) matter deeply.
Advertisement
For starters, the researchers found that using playful or childish terms in your day-to-day – “pee pee,” “hoo-ha,” “vajayjay” – tended to report more negative feelings about their genitals.
“These terms were also linked to a more negative perception of partner’s oral sex enjoyment, greater use of vaginal cleaning products and higher openness to labiaplasty,” said Tanja Oschatz, who studies women’s sexuality at Johannes-Gutenberg-University in Mainz, Germany, and co-authored the study.
Meanwhile, using vulgar terms during sex – “pussy,” “cunt” – is connected to a more positive sexual experience, Oschatz told HuffPost.
Advertisement
“Interestingly, using the word ‘pussy’ in sexual contexts was associated with greater sexual pleasure and more frequent orgasms,” she said. “This suggests that a word once considered derogatory may now be reclaimed by many women and carry an element of empowerment.”
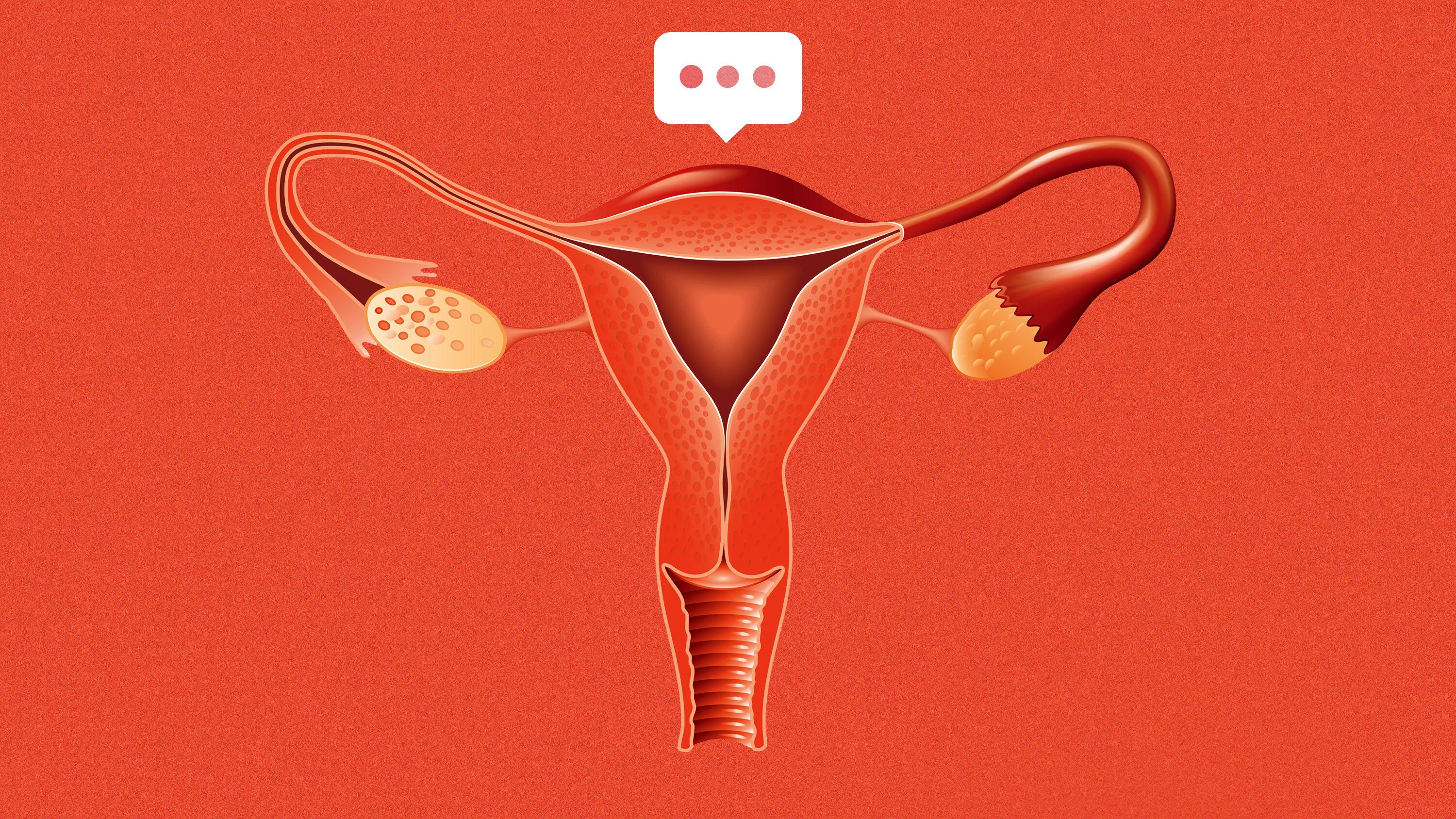
Illustration: HuffPost; Photo: Getty Images
For the study, recently published in the journal Sex Roles, researchers surveyed 457 women in the United States ranging in age from 18 to 81, with an average age of about 37.
Advertisement
The women were asked what terms they most commonly use to refer to their genitals in two different scenarios: everyday, non-sexual scenarios and during partnered sex.
Then, the women completed a series of questionnaires designed to assess their genital self-image, their overall sexual pleasure, orgasm frequency, attitudes toward oral sex and some health behaviours, like if they used vaginal cleaning products and their openness to labiaplasty, a type of cosmetic genital surgery meant to reshape or reduce the size of the labia minora or labia majora.
In everyday conversation, the study found that a majority of women, about 75%, reported using at least one anatomical term, with “vagina” being the most frequent. Playful euphemisms were also common, used roughly among 15% of the participants, especially older women. (So your mom isn’t the only one who blanches at the mention of “vagina.”)
Advertisement
There’s definitely been a generational shift in favoured terms, Oschatz said.
“One thing that was interesting was that compared to data from 20 years ago, we also found that the term ‘vulva’ (referring to the outer parts of women’s genitals) and words referring to the clitoris have become more common, suggesting a more differentiated and anatomically informed vocabulary today,” Oschatz said.
Context really mattered here, though. For instance, childish terms were linked to more negative attitudes only when used in non-sexual contexts, but not during sexual ones.
“We found that genital naming among women is very diverse,” Oschatz said.

Maskot via Getty Images
Advertisement
There’s a lot of discussion – especially in online parenting circles – about the need to use correct anatomical terms for genitalia. When kids feel comfortable saying “vagina” or “penis,” the argument goes, it reduces shame about their bodies and gives them the language they need to tell a trusted adult if someone touches them inappropriately.
While this study in no way discounts any of that – being intentional with our language and learning how to advocate for ourselves with our words is important – the study adds some nuance to our understanding of how that all plays out into adulthood.
The researchers were surprised to find that using euphemisms – vague and indirect terms like “down there” or “private area” – was not associated with more negative attitudes toward women’s own genitals.
Advertisement
“We had expected that these terms might carry an element of shame or discomfort, which could be linked to a more negative genital self-image. But our findings suggest otherwise. Instead, it was really the use of childish language that was related to negative feelings and attitudes,” Oschatz said.
With their study complete, Oschatz said she’s happy to see some researchers currently replicating their study in different cultures and languages. (Research really needs to be done on all those Brits calling it a “fanny”.)
“Language is so diverse it is likely that categories and connotations vary largely,” Oschatz said.